Electrodiagnostics
Overview
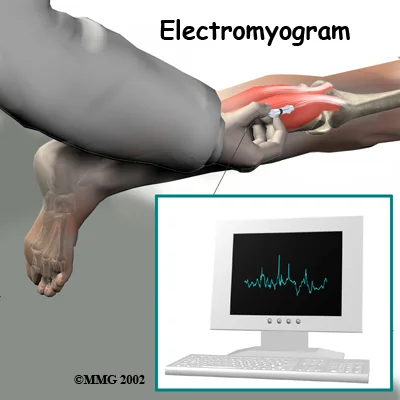
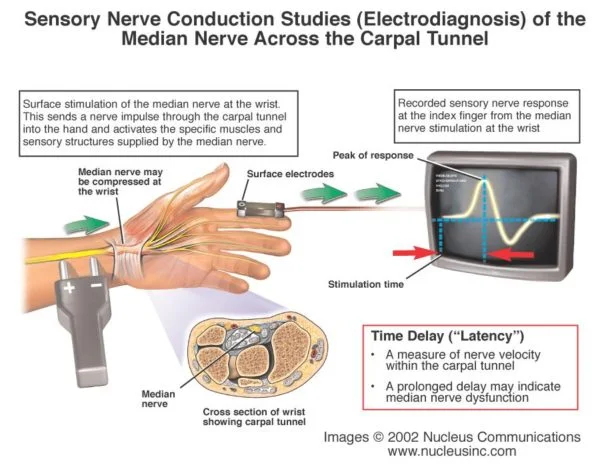
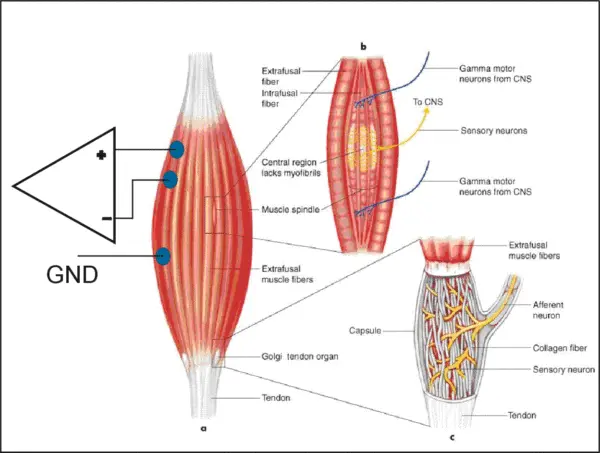
Electrodiagnostics (EDX) testing is used to evaluate the integrity and function of the peripheral nervous system (most cranial nerves, spinal roots, plexi, and nerves), NMJ, muscles, and the central nervous system (brain and spinal cord). EDX testing is performed as part of an EDX consultation for diagnosis or as follow-up of an existing condition. EDX studies can provide information to:
- Identify normal and abnormal nerve, muscle, motor or sensory neuron, and NMJ functioning.
- Localize region(s) of abnormal function.
- Define the type of abnormal function.
- Determine the distribution of abnormalities.
- Determine the severity of abnormalities.
- Estimate the date of a specific nerve injury.
- Estimate the duration of the disease.
- Determine the progression of abnormalities or of recovery from abnormal function.
- Aid in diagnosis and prognosis of disease.
- Aid in selecting treatment options.
- Assists in following response to treatment by providing objective evidence of change in neuromuscular function.
- Localize correct locations for injection of intramuscular agents (e.g., botulinum toxin).
Risks
During The Procedure
How Long Does EDX Take?
Carpal Tunnel Syndrome
Radiculopathy
Mononeuropathy and Polyneuropathy or Mononeuropathy Multiplex
Mononeuropathy
Polyneuropathy or Mononeuropathy Multiplex
Myopathy
Motor Neuronopathy
Plexopathy
Neuromuscular Junction
Timing of Testing After an Injury

Get Answers with Electrodiagnostics Nerve Tests
Frequency Of Electrodiagnostic Testing In A Given Patient
There are many clinical situations where good medical management requires repeat testing, such as in the following examples:
- Second diagnosis. Where a single diagnosis is made on the first visit, but the patient subsequently develops a new set of symptoms, further evaluation is required for a second diagnosis.
- Inconclusive diagnosis. When a serious diagnosis (e.g., ALS) is suspected but the results of the needle EMG/NCS examination are insufficient to be conclusive, 1, or even more, follow-up studies are needed to establish or exclude the diagnosis.
- Rapidly evolving disease. Initial EDX testing in some diseases may not show any abnormality (e.g., Guillain-Barré syndrome) in the first 1 to 2 weeks. An early diagnosis confirmed by repeat electrodiagnosis must be made quickly so that treatment can begin. Follow-up testing can be extremely useful in establishing prognosis and monitoring patient status.
- Course of the disease. Certain treatable diseases such as polymyositis and myasthenia gravis follow a fluctuating course with variable response to treatment. The physician treating such patients needs to monitor the disease progress and the response to therapeutic interventions. The results of follow-up evaluations may be necessary to guide treatment decisions.
- Unexpected course or change in course of the disease. In certain situations, management of a diagnosed condition may not yield expected results or new, questionably related problems may occur (e.g., failure to improve following surgery for radiculopathy). In these instances, reexamination is appropriate.
- Recovery from injury. Repeat evaluations may be needed to monitor recovery, to help establish prognosis, and/or to determine the need for and timing of surgical intervention (e.g., traumatic nerve injury).
Repeat EDX consultation is therefore sometimes necessary and, when justifiable, should be reimbursed. Reasonable limits can be set concerning the frequency of repeat EDX testing per year in a given patient by a given EDX consultant for a given diagnosis. The following numbers of tests per 12-month period per diagnosis per physician are acceptable:
- Two tests for carpal tunnel-unilateral, carpal tunnel-bilateral, radiculopathy, mononeuropathy, polyneuropathy, myopathy, and NMJ disorders.
- Three tests for motor neuronopathy and plexopathy.
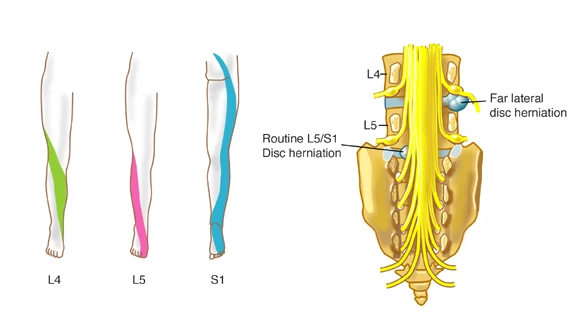
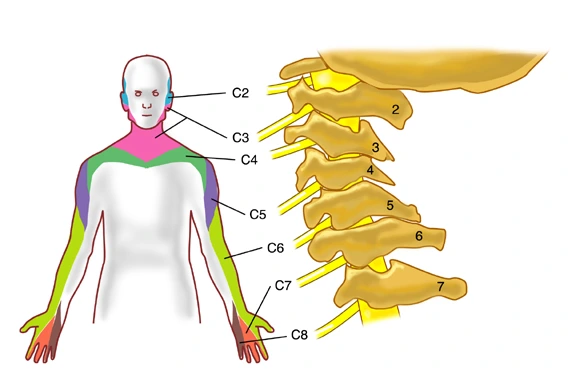
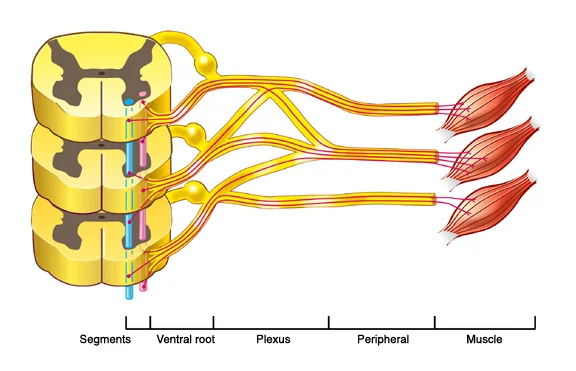
Spinal nerves have motor fibers and sensory fibers. The motor fibers innervate certain muscles, while the sensory fibers innervate certain areas of skin. A skin area innervated by the sensory fibers of a single nerve root is known as a dermatome. A group of muscles primarily innervated by the motor fibers of a single nerve root is known as a myotome. Although slight variations do exist, dermatome and myotome patterns of distribution are relatively consistent from person to person.
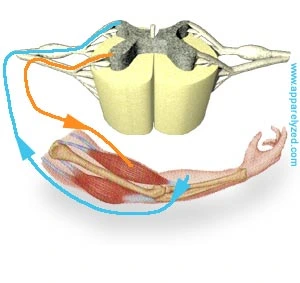
The ventral (anterior) gray matter of the spinal cord contains nerve cells that send axon fibers out, through the nerves, to their end points on the muscles that they activate. Sensory information from the body and arriving instructions from the brain all cause movement by giving instructions to these “motor neurons” in the spinal cord gray matter.
Spinal Cord Segmental Myotomes And Dermatomes
Myotomes
Each muscle in the body is supplied by a particular level or segment of the spinal cord and by its corresponding spinal nerve. The muscle, and its nerve make up a myotome. This is approximately the same for every person and are as follows:
- C3,4 and 5 supply the diaphragm (the large muscle between the chest and the belly that we use to breath).
- C5 also supplies the shoulder muscles and the muscle that we use to bend our elbow
- C6 is for bending the wrist back.
- C7 is for straightening the elbow.
- C8 bends the fingers.
- T1 spreads the fingers.
- T1 –T12 supplies the chest wall & abdominal muscles.
- L2 bends the hip.
- L3 straightens the knee.
- L4 pulls the foot up.
- L5 wiggles the toes.
- S1 pulls the foot down.
- S3,4 and 5 supply the bladder. bowel and sex organs and the anal and other pelvic muscles.
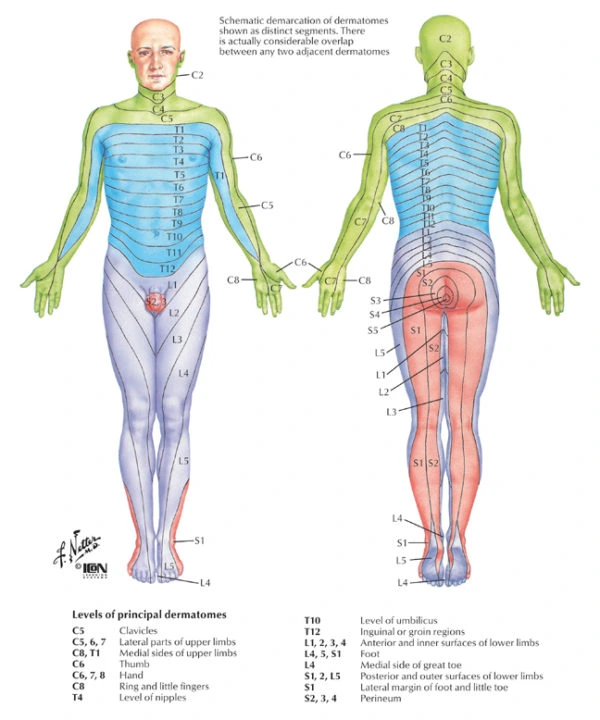
Spinal Cord Segmental Dermatomes