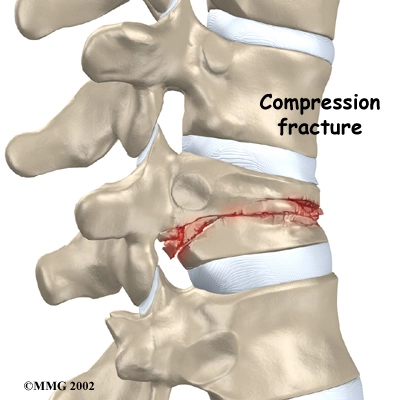
Vertebroplasty For Compression Fractures
Overview

Restore Stability In Your Spine With Vertebroplasty
Factors that increase the likelihood of developing osteoporosis include:
- Being female
- Being thin or having a small frame
- Advanced age
- A family history of osteoporosis
- Being past menopause
- Abnormal absence of menstrual periods
- Anorexia or bulimia
- A diet low in calcium
- Long-term use of medications such as corticosteroids or anticonvulsants
- Lack of exercise
- Smoking
- Excessive use of alcohol
Bone tumors and metastatic bone disease also lead to vertebral compression fractures. Diseases such as multiple myeloma and hemangioma (types of tumors) place patients at great risk for these painful fractures. High doses of steroids for the control of auto-immune diseases such as lupus and rheumatoid arthritis, as well as asthma or chronic pulmonary disease can also increase the risk of reduced bone mass and resulting fractures.
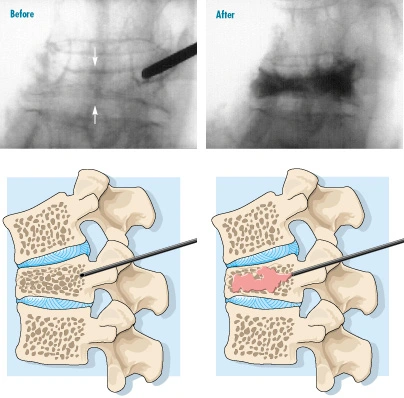
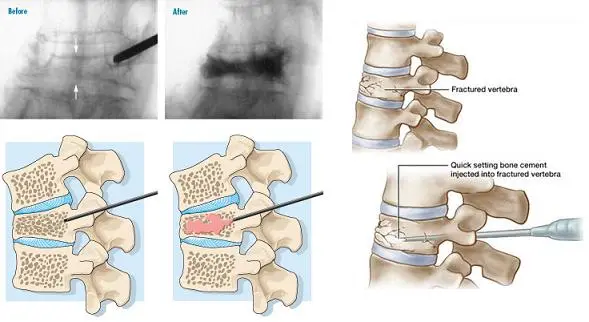
Percutaneous vertebroplasty may be done either as an inpatient or outpatient procedure, depending upon the severity of the fracture and the health of the patient. After suitable sedation is given, a needle is placed into the affected vertebra and fills the damaged area with bone cement.
In many patients, the pain is lessened or even gone within 24 hours. There are few side effects or problems. In some cases, increased pain and fever may occur for a short time. This is treated with anti-inflammatory drugs. Other risks to the patient include infection and allergic reactions to x-ray dye or other medications. There is a very small risk that the cement could leak into areas outside of the vertebra at the time of the procedure, causing spinal cord or nerve damage.
If leakage occurs, surgery could be required and the patient could have permanent nerve and organ injury.
Pre-Operative Preparation
During the Procedure
After the procedure
You must lay flat after the procedure. You will need to follow-up in the clinic after five to ten days. Keep the area clean and dry to help prevent skin infection. Do not do any heavy lifting for 3 months (i.e. nothing heavier than a carton of milk). After that, you can gradually increase your lifting to normal. Walking is encouraged and you can bend within the restrictions of your brace. You may experience some muscle discomfort where the needles were placed. This may be treated with a mild pain reliever such as Tylenol. Do not drive for the remainder of the day. Please have an adult drive you home or accompany you in a taxi or other public transportation. Depending on how you feel, you may resume normal activities and return to work the next day.
Benefits: Immediate Relief from Pain, Improved Quality of Life
What are the risks of Vertebroplasty?
The risks are minimal and in fact, few complications have been reported involving less than five percent of cases. As with any procedure, there is a risk of significant complications. The most common side effects from the nerve root block can include (but are not limited to):
- Allergic reactions to medications.
- Infection (occurs in less than 1 per 15,000 injections).
- Post-injection flare (nerve root irritation with pain several hours after treatment, which may last days or weeks).
- Depigmentation (a whitening of the skin).
- Local fat atrophy (thinning of the skin).
- Destruction of a motor or sensory nerve in the path of the needle.
- Bleeding, nerve injury, organ injury and death are rare but possible.
- Cement leakage is possible. The cement used in vertebroplasty is in a liquid form and is squeezed into the fractured vertebra under high pressure. Some of the cement commonly leaks out of the vertebra, but this usually doesn’t cause any problems. Only rarely does a cement leak cause pressure on the spinal cord or nearby nerves. In these cases, surgery may be required to remove the pressure.
- Ongoing pain may occur. Many patients get nearly complete relief of symptoms from vertebroplasty. As with any procedure, however, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your doctor about treatments that can help control your pain.
